Systematic review and meta-analysis looks at the adverse effects of CBD across all medical indications.
Introduction
Cannabidiol (CBD) has been approved by both the US Food and Drug Administration (FDA) and European Medicines Agency (EMA) as an add-on treatment for two rare childhood epilepsies: Dravet Syndrome and Lennox-Gastaut Syndrome [1]. Recent clinical trials have also examined CBD as a potential treatment for diabetes [2], fatty liver disease [3] and schizophrenia [4]. CBD is also available in over-the-counter (OTC) preparations which have not been evaluated in clinical trials [5]. To date, most clinical trials of CBD have involved 99% pure CBD at doses of 300–1500 mg/day. OTC preparations typically contain CBD along with other cannabinoids, and provide doses of 5–20 mg/day. However, some OTC preparations reportedly contain much higher or lower quantities of CBD while the market is poorly regulated and many products are mislabeled [5].
The precise molecular mechanism of action of CBD is unclear. Its effects have been related to the inhibition of fatty acid amide hydrolase, inhibition of adenosine reuptake, agonism of transient receptor potential channels, antagonism of the orphan G-protein-coupled receptor GPR55, facilitation of 5-HT1A mediated neurotransmission, and inhibition of inflammatory cytokines via action at receptors such as peroxisome proliferator-activated receptor-gamma [6,7,8,9]. It has a low affinity for cannabinoid (CB) receptors, but may act as a negative allosteric modulator at the CB1 receptor [10].
CBD has a reputation for having few adverse effects [11], and this is consistent with data from clinical trials [2,3,4]. Previous reviews of the safety and tolerability of CBD did not include meta-analyses [12, 13], included data from other cannabinoids [14], or were limited to studies in epilepsy [15]. Given the recent approval of CBD by the FDA and EMA for childhood epilepsy syndromes, and the wide range of other indications for which it is being marketed, a quantitative assessment of its safety and tolerability is timely. The aim of the present study was to address this issue by conducting a systematic review and meta-analysis of the adverse effects of CBD across a range of indications.
Methods
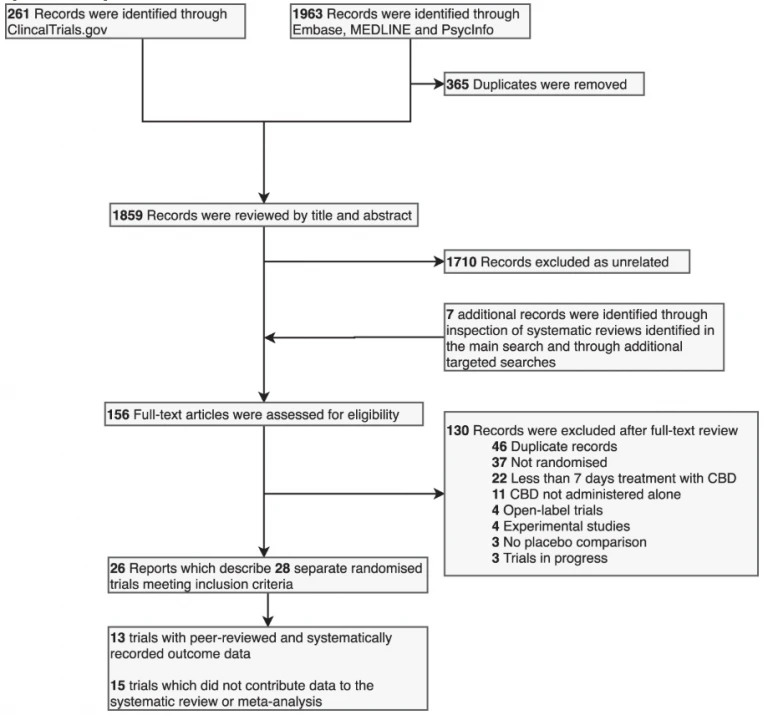
This systematic review and meta-analysis was prospectively registered on PROSPERO (CRD42018111429) and reported according to the PRISMA statement. The PRISMA flowchart is shown in Fig. 1.
Fig. 1: PRISMA Flow Diagram.
Inclusion and exclusion criteria
We included double-blind randomized controlled clinical trials that reported data on withdrawal, serious adverse events or adverse events from placebo-controlled trials of CBD in humans. Studies that were open-label, did not include a placebo comparison, were quasi-randomized, or lasted < 7 days were excluded. There were no restrictions in relation to participant characteristics or disease indication.
Search strategy
We searched Embase, MEDLINE, PsycInfo, and ClinicalTrials.gov. For Embase, MEDLINE, PsycINFO we used the keyword search term ‘(CBD OR cannabidiol) AND trial’. For ClinicalTrials.gov we searched for completed studies with the terms ‘cannabidiol OR CBD’. Each database was searched from its inception until 31/01/2019. We supplemented this search by reviewing the references of papers and systematic reviews identified in the search.
Two reviewers (EC and AG) independently screened the titles and abstracts of all articles identified by the search. The full texts of those selected were then reviewed by two independent authors (EC and AG). Any disagreements were resolved after discussion with a third author (DO).
Data extraction
Two authors (from SS, AG and EC) independently extracted outcome data on withdrawals, serious adverse events and adverse events from each study. Systematically recorded data were extracted from studies that had been published in a peer-reviewed journal or reported on ClinicalTrials.gov; data from posters, abstracts and other informal reports that had not been subject to peer review were excluded. If a study reported both treatment-related adverse events and adverse events we preferentially extracted adverse events, to reduce the risk of unanticipated adverse events being inadvertently disregarded. If two or more reports of the same study contained conflicting data, we preferentially used the data reported on ClinicalTrials.gov. The two sets of extracted data were then compared and any differences were resolved by a third author (EC or DO). Synonymous outcome measures were combined (by EC and DO) and are described in Table S2.
Bias assessment
Each study was assessed for bias using the Cochrane Risk of Bias Tool, which includes the following criteria: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, other bias [16]. Each criterion was rated as being at high, low, or unclear risk of bias by two independent raters (AG and SS). Disagreements were resolved after discussion with a third author (EC or DO).
Statistical analysis
We conducted a pairwise meta-analysis of all outcomes for CBD vs. placebo where more than eight events were recorded across both arms of all studies. As all outcomes were dichotomous, we calculated odds ratios (OR) with 95% confidence intervals using the Mantel–Haenszel method, where an OR > 1 indicates an increased likelihood of the event when treated with CBD compared with placebo and an OR below 1 indicates a reduced likelihood.
To convert mg/kg into a comparable daily dose we multiplied doses by 70 kg. Subgroup analyses of epilepsy studies and non-epilepsy studies were completed. Random-effects models were used to control for heterogeneity and we completed meta-regression analyses of CBD dosage. In such cases, data from the placebo arm were divided by the number of CBD arms contributing data to the meta-regression. Risk of publication bias was tested with the Egger regression intercept method and visual inspection of funnel plots. The significance level was set to p < 0.05 (two tailed). Pairwise analyses were conducted using Review Manager Version 5.3. Meta-regression analyses and publication bias analyses were conducted using Comprehensive Meta-Analysis Version 3.
Results
Identification of studies
The systematic search identified 28 independent randomized double-blind placebo-controlled clinical trials (Fig. 1), comprising data from a total of 1589 participants. Ten studies were excluded from further analysis because they were only reported in abstracts, posters or secondary descriptions from the grey literature. A further five were excluded because they did not report data on withdrawal or adverse events in a systematic way. The remaining 13 trials included a total of 822 participants and reported 266 different adverse outcomes, of which 33 provided sufficient data for meta-analysis (i.e., at least eight events across arms across studies per outcome) (Table 1). One study [3] met all the inclusion criteria but none of the events it reported occurred in outcomes relevant to the meta-analysis. It contributed data to estimates of event rates but did not contribute data to the calculation of OR. This meant that 12 trials using data from 803 participants contributed data to the meta-analysis. The studies that were not included are described in Table S1.
Table 1 Characteristics of included studies.
Of the 13 studies included in the systematic review, 5 involved patients with epilepsy and 2 involved patients with schizophrenia. The remaining six studies involved subjects with problematic cannabis use, Huntington’s disease, type II diabetes, non-alcoholic fatty liver disease, Crohn’s disease and healthy volunteers. The duration of treatment ranged from 1 to 14 weeks, and the dose of oral CBD ranged from 200 to 3000 mg per day. The mean oral dose used was 1132 mg/day and the median dose was 1200 mg/day. One study used sublingual CBD at a dose of 20 mg/day. In epilepsy studies the mean oral dose was 1214 mg/day; in non-epilepsy studies the mean oral dose was 918 mg/day. All trials are believed to have used pure, pharmaceutical-grade CBD, with minimal other cannabinoids.
Meta-analysis
We report on our primary outcome measures below, together with any secondary outcome that achieved statistical significance (p < 0.05) (Fig. 2) and subgroup analyses of epilepsy and non-epilepsy studies (Figs. 3 and 4). Non-significant secondary outcomes are described in Table S4.
Fig. 2: Summary of meta-analysis results: all studies.
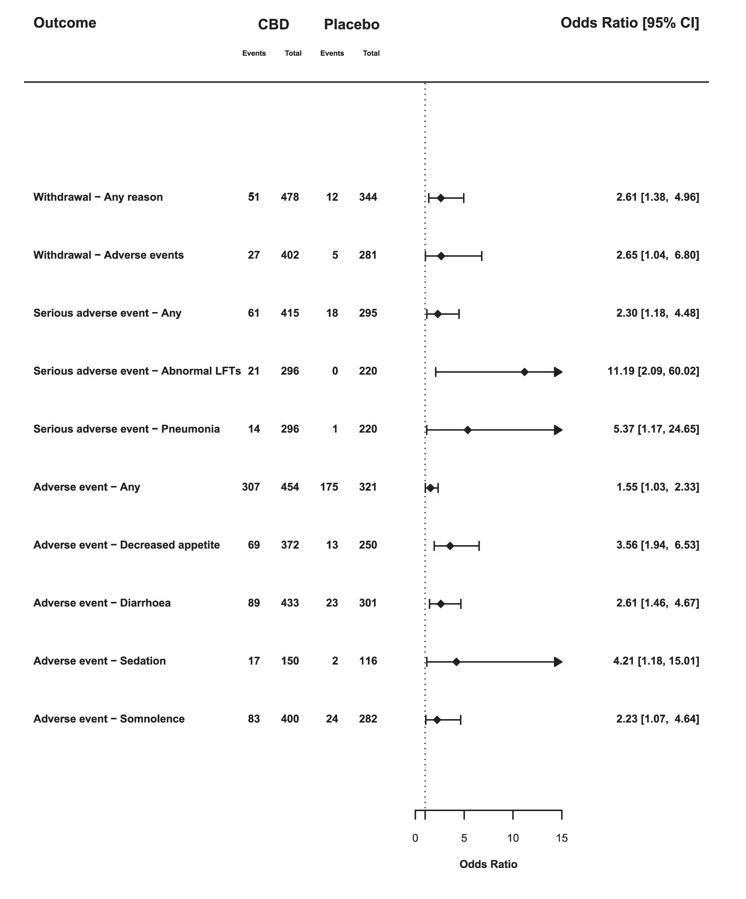
Odds ratios and 95% confience intervals (CIs) comparing CBD with placebo on outcomes which achieved statistical significance (p < 0.05). OR > 1 indicates an increased likelihood of the event when treated with CBD compared with placebo and an OR below 1 indicates a reduced likelihood. Abbreviations: LFTs, liver function tests.
Fig. 3: Summary of subgroup analyses: epilepsy studies.
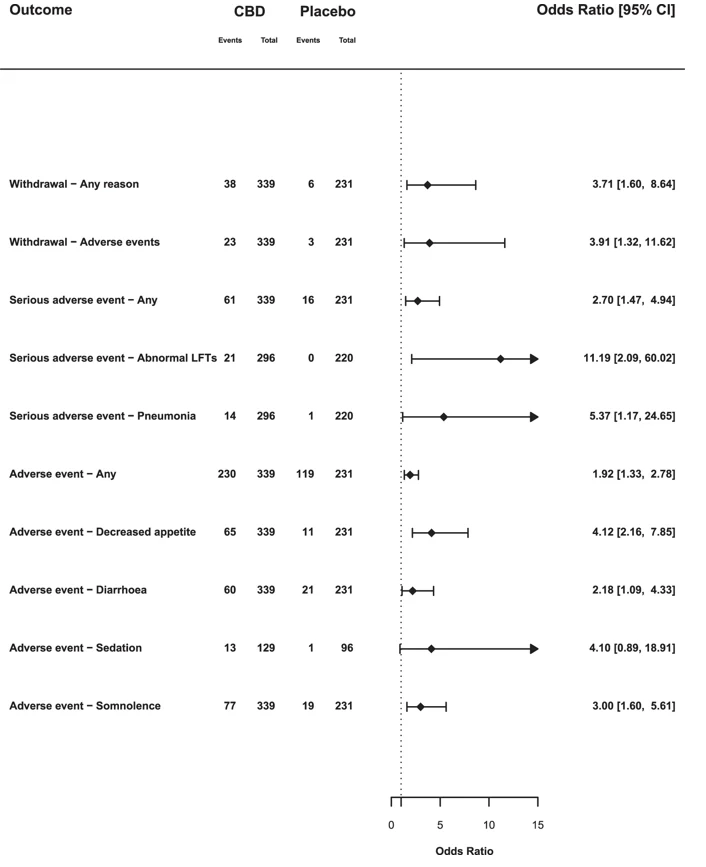
Odds ratios and 95% confience intervals (CIs) comparing CBD with placebo for selected outcomes from studies in childhood epilepsy syndromes. OR > 1 indicates an increased likelihood of the event when treated with CBD compared with placebo and an OR below 1 indicates a reduced likelihood. Abbreviations: LFTs, liver function tests.
Fig. 4: Summary of subgroup analyses: non-epilepsy studies.
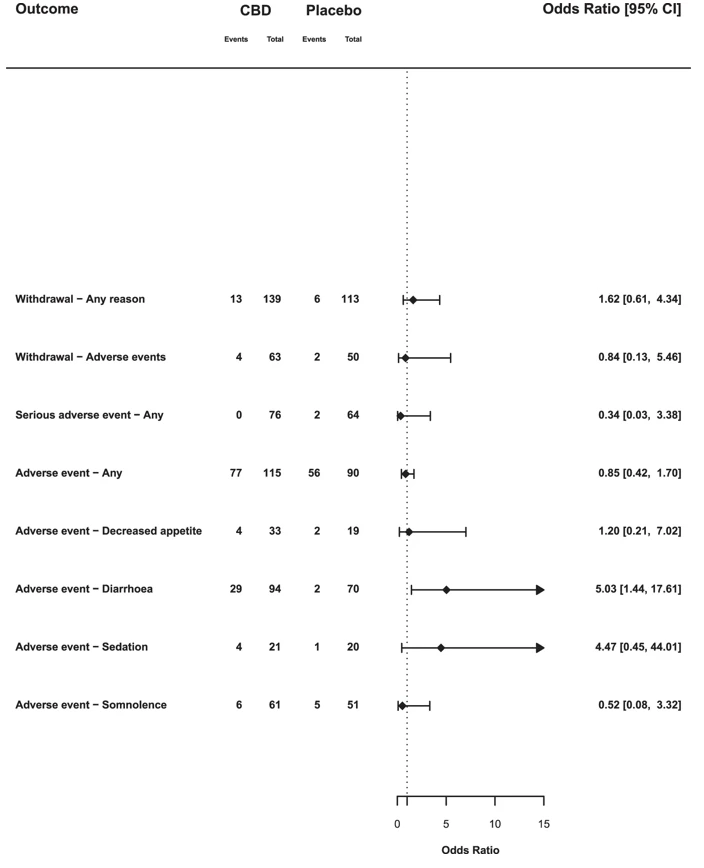
Odds ratios and 95% confience intervals (CIs) comparing CBD with placebo for selected outcomes from non-epilepsy studies. OR > 1 indicates an increased likelihood of the event when treated with CBD compared with placebo and an OR below 1 indicates a reduced likelihood.
Withdrawal
Across all doses, there were more withdrawals due to any reason (OR 2.61, 95% CI: 1.38–4.96) in CBD groups compared with placebo. The likelihood of withdrawal appeared to depend on the dose of CBD. At high doses (1400–3000 mg) 12.9% (35/272) of participants withdrew, compared with 8.8% (14/160) at medium doses (600–1000 mg), and only 4.3% (2/46) at low doses (20–400 mg), a similar rate to placebo (3.5% [12/344]). Meta-regressions indicated that there was a trend for an effect of CBD dose on withdrawal (β = 0.0014; p = 0.077). Withdrawal due to adverse events was also higher in CBD groups compared with placebo (OR 2.65, 95% CI: 1.04–6.80), although there was no significant correlation with CBD dose in the meta-regression (β = 0.0014; p = 0.274).
In studies of patients with rare epilepsy syndromes there was an increased odds of withdrawal due to any reason (OR 3.71, 95% CI: 1.60–8.64), and withdrawal due to adverse events (OR 3.91, 95% CI: 1.32–11.62). However, in non-epilepsy studies withdrawal due to any reason (OR 1.62, 95% CI: 0.61–4.34) or adverse events (OR 0.84, 95% CI: 0.13–5.46) was no more common than with placebo.
Serious adverse events
There were 61 serious adverse events in 415 participants in the CBD arms (14.7%), compared with 18 among 295 participants in the placebo arms (6.1%), an OR of 2.30 (95% CI: 1.18–4.48). The result of the dosage meta-regression was not significant (p = 0.169). In epilepsy studies the OR was 2.70 (95% CI: 1.47–4.94), in non-epilepsy studies it was 0.34 (95% CI: 0.03–3.38). This results from serious adverse events associated with CBD treatment being limited to studies in children with epilepsy.
There was an increased OR for pneumonia (OR 5.37, 95% CI: 1.17–24.65). This reflected 14 cases of pneumonia recorded as a serious adverse event in patients treated with CBD, compared with only 1 in placebo arms. An additional two cases of pneumonia were recorded as (non-serious) adverse events in patients treated with CBD in another study [17]. However, pneumonia was only reported in studies of children with epilepsy.
There was an increased OR for abnormal liver function tests (OR 11.19, 95% CI: 2.09–60.02), with all 21 events occurring in the CBD groups compared with no events in patients treated with placebo. These differences were only evident in studies involving childhood epilepsy, and most of the events (19 of 21) occurred when CBD was given at high doses (20 mg/kg or more). Each of the three trials contributing data to this outcome used a cut-off of >3 times the upper limit of normal for transaminase increases.
Adverse events
The OR for experiencing any adverse event with CBD compared with placebo was 1.55 (95% CI: 1.03–2.33). In total, 67.6% of CBD-treated participants reported an adverse event, compared with 54.5% of those treated with placebo. Here, the results of dosage meta-regression were highly significant (β = 0.0013, p = 0.0023): the likelihood of an adverse event was strongly related to the dose of CBD. The likelihood of adverse events also differed according to the clinical group being treated (χ2 = 4.17; p = 0.04). In the five studies involving children with epilepsy, 67.8% of those given CBD had adverse events, compared with 51.5% on placebo (OR 1.92, 95% CI: 1.33–2.78), whereas in the five non-epilepsy studies the rates were similar: 67.0% and 62.2%, respectively (OR 0.85, 95% CI: 0.42–1.70).
CBD was also associated with a greater OR for decreased appetite (OR 3.56, 95% CI: 1.94–6.53), diarrhoea (OR 2.61, 95% CI: 1.46–4.67), sedation (OR 4.21, 95% CI: 1.18–15.01) and somnolence (OR 2.23, 95% CI: 1.07–4.64). In epilepsy studies, CBD was associated with decreased appetite (OR 4.12, 95% CI: 2.16–7.85), diarrhoea (OR 2.18, 95% CI: 1.09–4.33) and somnolence (OR 3.00, 95% CI: 1.60–5.61). Sedation (OR 4.10, 95% CI: 0.89–18.91) was not statistically different from placebo (p = 0.07). In non-epilepsy studies, the only event that was more frequent with CBD was diarrhoea (OR 5.03, 95% CI: 1.44–17.61).
Other outcomes
All other outcomes were non-significant (p > 0.05; Table S4).
Risk of bias
Ten studies were rated as having a low risk of bias [2,3,4, 17,18,19,20,21,22,23], one was rated as having an unclear risk of bias [24], and two studies were rated as having a high risk, due to selective outcome reporting [25, 26]. Results of the risk of bias assessment are described in Table S3.
Discussion
To our knowledge, this is the first systematic review and meta-analysis of the adverse effects and tolerability of CBD across all indications. We identified a total of 28 trials, of which 13 met inclusion criteria and 12 provided suitable data for meta-analysis from a total of 803 participants. Our main findings were that although CBD was associated with a greater likelihood of adverse events and study withdrawal, this was almost entirely specific to studies in rare forms of epilepsy. These differed from the others we examined, in that they involved relatively high doses of CBD in children, many of whom were also being treated with other anti-epileptic medications.
CBD is a potent inhibitor of the CYP450 enzymes, CYP3A4 and CYP2C19. These hepatic enzymes metabolize clobazam and sodium valproate, which were prescribed in over half of the patients in the three main epilepsy studies included in the meta-analysis [17, 18, 27]. Inhibition of CYP2C19 can increase the levels of clobazam’s metabolite, N-desmethylclobazam, by two- to seven-fold, which has a significant sedative effect [28]. In a recent experimental study, even very high acute doses of CBD (1.5 and 4.5 g orally) had limited effects on alertness, suggesting that CBD alone is not usually sedative [29]. Increased N-desmethylclobazam levels could also account for the increased odds of pneumonia in epileptic patients taking CBD, as this increases the risk of sedation, respiratory depression and aspiration [30]. Again, these events only occurred in patients prescribed high doses of CBD (10–20 mg/kg/day). It is less clear if CBD interacts with clobazam at lower doses, although it has been reported that CBD inhibits CYP2C19 at doses of 5 mg/kg [31], and therefore has the potential to interact with a wide range of other commonly prescribed medications even at low-medium doses. The majority of cases with abnormal liver function tests were in children with epilepsy who were also being treated with sodium valproate. The exact mechanism of this interaction is not fully understood. Co-administration of CBD and valproate does not significantly alter their plasma levels or that of their metabolites [32]. However, the metabolite 7-COOH-CBD, valproate and its metabolite 4-ene-valproic acid may affect hepatic mitochondrial function [33].
An increased incidence of diarrhoea in CBD-treated individuals is consistent with data from a small experimental study, which found that single doses of CBD, 1.5 g and 4.5 g, produced diarrhoea in 10% and 20% of participants, respectively [29]. This may reflect the endocannabinoid system’s role in the regulation of gastrointestinal motility [34]. CBD treatment was also associated with reduced appetite in the epilepsy studies. The endocannabinoid system contributes to the regulation of food intake and moderates the hedonic effect of food consumption [35]. Previous studies have suggested that CBD in cannabis may reduce the appetitive effects of food stimuli [36], but its molecular mechanism of action in this context remains unclear. Rimonabant, a selective inverse agonist at the CB1 receptor, reduces appetite and weight and was approved as a treatment for obesity before being withdrawn because of adverse psychiatric side effects [37]. Dronabinol, a synthetic form of THC, and a partial agonist at CB receptors, has been used as a treatment for anorexia and cachexia in HIV and cancer [38, 39]. In the trials identified by our systematic search, weight was monitored too infrequently to be evaluated.
Strengths of the present study include its pre-registered protocol, comprehensive systematic search strategy, and its timeliness as the first meta-analysis of the safety and tolerability of CBD across all indications. The overall quality of studies included was high and it is unlikely that a significant amount of bias was introduced. Publication bias is also unlikely to have inflated summary ORs, as our target outcomes were not the primary outcome measure, nor the desired outcomes for the studies we examined. Many studies in our systematic review were excluded from the meta-analysis because they did not report adverse events systematically or had not been peer-reviewed. The meta-analysis therefore only contained data from 803 participants, reducing its power to identify uncommon adverse events. We included studies across a range of treatment indications which aids generalizability to different patient groups in clinical practice. However, most (69%) of the participants in our meta-analysis had childhood epilepsy. This is an important consideration, as these studies involved children rather than adults, relatively high doses of CBD, and the patients were often taking other epilepsy medications which can interact with CBD. Although we were able to stratify our analysis to investigate differences between the studies on epilepsy and on other indications, there is a need for further studies that include a broader range of patient groups and indications.
A key consideration in interpreting our findings is that the doses of CBD used in the trials we studied were relatively high (median dose 1200 mg/day; mean dose 1132 mg): only 46 of 822 participants received doses at or below 400 mg/day or 5 mg/kg/day [2, 3, 21, 25]. The doses of CBD provided by health and food supplements are typically much lower (5–20 mg/day [5]), so the incidence of adverse events is likely to be lower. However, this has yet to be demonstrated. This issue requires more research, as the commercial CBD market is poorly regulated. At present, some OTC products are poorly labelled, others do not contain purified CBD, and many contain other cannabinoids or contaminants in addition to CBD [40, 41].
Conclusions
CBD is well tolerated and has few adverse effects. However, its ability to inhibit the hepatic metabolism of other medications (such as clobazam and sodium valproate) has the potential to cause adverse effects. This is demonstrated by the increased rates of adverse events, serious adverse events and withdrawals in trials for childhood epilepsy syndromes but not other indications. Additional safety data from clinical trials outside of childhood epilepsy syndromes and from studies of OTC CBD products would be beneficial.
Funding and disclosure
The authors declare no competing interests.
Link to source:
Adverse effects of cannabidiol: a systematic review and meta-analysis of randomized clinical trials.

